DS vs RNY statistics
This is a comparison from two papers of the long-term results with the RNY and DS. The RNY study (Shah et al.) can be found at http://jcem.endojournals.org/cgi/content/full/91/11/4223, and the Hess study was published in Obesity Surgery, 15, 408-416 (2004) (I have a .pdf copy if anyone wants to have it).
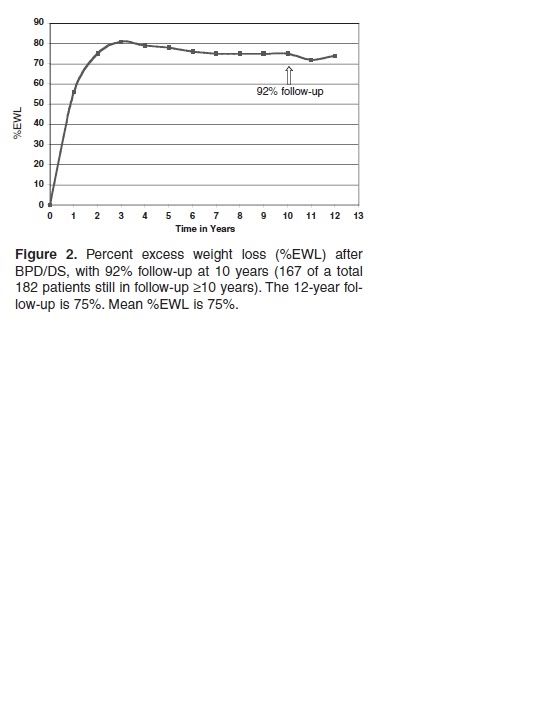
Even if the curves are oppositely oriented, and one measures percent weight change, and the other percent excess weight lost, and even if you assume that both DSers and RNYers end up at the same initial maximum EWL% (which isn't the case), the curves are pretty directly comparable. The first is from the Shah study; the second is from the Hess study.

FIG. 1. Weight changes among subjects participating in the Swedish Obese Subjects study over a 10-yr period (11 ). There were 627 control subjects who did not undergo bariatric surgery, 156 who underwent banding, 451 who underwent vertical banded gastroplasty, and 34 who had gastric bypass.
Also, there is this study from Christou, reporting long-term RNY results: http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pub med&pubmedid=17060766
in which he reports:
There was a significant increase in failures and decrease in excellent results at 10 years when compared with 5 years. The failure rate when all patients are followed for at least 10 years was 20.4% for morbidly obese patients and 34.9% for super obese patients. CONCLUSIONS: The gastric bypass limb length does not impact long-term weight loss. Significant weight gain occurs continuously in patients after reaching the nadir weight following gastric bypass. ************************ Here are some comments from the bariatric surgeons hired by CHDR (see below) *****view appeals of patients who want the DS over the RNY, copied from the California Department of Managed Health Care's decisions: http://tinyurl.com/o4js9
A 60-year-old female enrollee has requested for laparoscopic biliopancreatic diversion with duodenal switch (DS) for treatment of her morbid obesity. Findings: The physician reviewer found that with a BMI of 43.2 and multiple comorbid conditions, the patient met nationally accepted medical necessity criteria for consideration of weight loss surgery. Peer reviewed articles clearly demonstrate superior weight loss and maintenance of weight loss over the long term with the DS as compared to other surgical procedures. Published data also demonstrates that the Roux-en-Y procedure results in as much, if not more, protein calorie malnutrition as the DS. The patient’s assertion that the DS is the most effective surgical weight loss alternative is well supported in the literature and this option was a medically reasonable approach to surgical weight loss. Psychological, nutritional and cardiology evaluations indicated the patient was an appropriate candidate for the surgery.
A 44-year-old female enrollee has requested bariatric surgery including duodenal switch and laparoscopic cholecystectomy for treatment of her morbid obesity. Findings: The physician reviewer found that this patient clearly meets the criteria set by the National Institutes of Health for surgical treatment of obesity. The question raised relates to what would be the best surgical approach. Serious consideration should be given to the medications the patient is likely to take the rest of her life for her SLE and associated joint pain. Specifically, NSAIDs, Methotrexate, Plaquenil, and potential high-dose steroids with exacerbation of SLE symptoms. These medications can predispose the patient to ulcer formation and other gastrointestinal complaints. In comparing the duodenal switch procedure to the standard Roux-en-y gastric bypass, the literature indicates that the duodenal switch has proven to be superior with regard to gastritis, marginal ulcer formation, dumping syndrome, nutritional abnormalities and the stability of the weight loss.
There are many more such statements in the many MANY decisions overturning insurance company denials of the DS on this site. Please have a look.
Regarding CHDR: http://www.maximus.com/corporate/pages/CHDR.asp:
MAXIMUS CHDR is the nation’s leading independent medical reviewer of disputed health insurance claims. CHDR serves more than 25 states in the role of reviewer of appeals made by health plan enrollees. We also are the official Medicare Managed Care Independent Review Entity for the Federal Centers for Medicare & Medicaid Services (CMS). We serve in a similar capacity for the federal Office of Personnel Management (OPM), reviewing claims disputes in connection with the Federal Employee Health Benefits Program (FEHBP).
So you can imagine that Medicare and FEHBP would engage a relatively conservative reviewing agency, to appease their insurance companies -- but their bariatric surgeons believe the DS is best. Go figure. ***************************** From the Shah paper http://jcem.endojournals.org/cgi/content/full/91/11/4223 (relates primarily to RNY and GB [gastric banding):
| Effect of Bariatric Surgery on Nutritional Status and Intolerance |
|---|
Micronutrient deficiency
Deficiency of iron, vitamin B12, folate, calcium, and vitamin D has been frequently observed after RYGB surgery. Deficiency of vitamin A has also been observed, although less frequently. Nutrient deficiencies after GB surgery are less common because it does not have a malabsorptive component, and an adult multiple vitamin and mineral supplement is considered sufficient to prevent these problems (64). Reviewed below are the studies that have reported nutritional deficiencies in RYGB surgery patients (Table 2![]() ). The majority of these studies were uncontrolled case series, and so it is important to note that the studies may have somewhat overestimated the effect of surgery on nutritional status, especially given that nutritional deficiencies have been noted in severely obese subjects before surgery (65) and that many of the patients are menstruating women who are more likely to have poor iron status.
). The majority of these studies were uncontrolled case series, and so it is important to note that the studies may have somewhat overestimated the effect of surgery on nutritional status, especially given that nutritional deficiencies have been noted in severely obese subjects before surgery (65) and that many of the patients are menstruating women who are more likely to have poor iron status.
|
Serum iron deficiency is seen frequently in RYGB patients (66, 67, 68, 69), with the incidence rate as high as 52% (66). The incidence of anemia (type not specified) has been reported to be as high as 74% (66). Supplements containing usual daily doses of multivitamins (70), and even high doses of oral iron (320 mg twice daily) (71), do not consistently prevent anemia in menstruating women. Contributing factors to iron deficiency anemia include malabsorption due to bypassing of the duodenum and proximal jejunum, the main sites for iron absorption (Fig. 2
|
Vitamin B12 deficiency, assessed by serum vitamin B12 levels, is also frequently seen in RYGB patients (66, 67, 68, 69, 73) with the incidence rate as high as 64% (67). Most vitamin B12 deficiencies in RYGB patients may be corrected by 500 µg/d oral B12 supplementation (74), and a minimum dose of 300 µg crystalline B12 per day is necessary to maintain normal serum levels (75). Only a small number of patients require parenteral administration of B12 (2000 µg/month) (64). Possible factors that contribute to B12 deficiency include achlorhydria (72), which prevents its cleavage from foods; decreased consumption due to intolerance to its main sources (milk and meat) (15); and poor secretion of intrinsic factor needed for its absorption (73). Because of the latter problem, Elliot (64) recommended taking the supplement in a sublingual form.
Serum folate deficiency has been reported to be as high 38% after RYGB surgery (67). Brolin et al. (74) reported that a supplement containing 400 µg of folate per day consistently corrected low folate levels in patients who underwent RYGB surgery, although 1000 µg/d have been recommended by others (64). Primary reason for folate deficiency is decreased folate intake. Malabsorption may not play a big role, even though folate is preferentially absorbed in the proximal part of the small intestine, because absorption can occur along the entire part of the small intestine with adaptation after surgery (76). Maintaining adequate folate levels is important, however, because of the possibility of megaloblastic anemia. Also, there have been reports of neural tube defects in infants born to mothers who underwent RYGB surgery (77, 78).
Calcium and vitamin D deficiency may occur in patients who undergo RYGB surgery, and a deficiency rate of 10% for serum calcium and 51% for serum 25-hydroxy vitamin D levels has been reported (66). PTH levels, however, were not reported (66). Possible contributors to calcium deficiency in the RYGB patients include malabsorption of calcium because of bypassing the duodenum and proximal jejunum in which calcium is mostly absorbed; intolerance to rich sources of calcium such as milk; and defective absorption of vitamin D because of fat malabsorption. Fat malabsorption is due to the short common channel and delayed mixing of fat with pancreatic enzymes and bile salts as a result of bypassing the duodenum. Deficiency of calcium is not always apparent, however, because of release of calcium from bone. Coates et al. (79) and von Mach et al. (80), who followed subjects for 9 and 24 months, respectively, reported elevated markers of bone turnover and/or decreased bone mass in patients who underwent RYGB surgery, compared with patients who underwent GB surgery (80) or the matched obese controls (79, 80). The higher bone turnover in the RYGB patients, however, may be partly due to the increased weight loss in these patients, compared with the other patients. PTH levels were not different between the RYGB and obese control groups (80) nor did they change over time after surgery (79). Nevertheless, to prevent metabolic bone disease, 1200–1500 mg/d of calcium and 400 IU/d of vitamin D supplements are recommended (64, 65). These amounts, however, may not suppress serum PTH or bone resorption, and increased supplementation may need to be considered (81). Because of reduced stomach acid content, calcium citrate rather than calcium carbonate is recommended because the latter requires acid for absorption (64, 65). Regular monitoring of markers of bone resorption such as urinary N-telopeptide level and markers of bone formation such as serum osteocalcin level may also be necessary.
Serum vitamin A deficiency has been reported in 10% of RYGB patients (66, 67). Whereas symptoms of vitamin A deficiency are rare in this population, a case study reported xerophthalmia and nyctalopia in a patient after a duodenal switch gastric bypass surgery due to inadequate vitamin A supplementation (82). A contributing factor to vitamin A deficiency in RYGB patients is fat malabsorption. Careful monitoring of serum vitamin A status and supplementation as needed is necessary to avoid a deficiency.
Despite the evidence of nutritional deficiencies, many surgeons do not recommend adequate supplements or evaluate serum nutrient levels (83), and most patients do not comply with the recommended supplement regimen (70). Education of both the physicians and patients is thus necessary to prevent malnutrition after RYGB surgery.
Macronutrient deficiency and intolerance
Protein deficiency, assessed by serum albumin levels, is less common than most other nutrient deficiencies (Table 2![]() ) (66, 67, 68, 69). To consume enough protein, patients should be advised to consume fish, which is better tolerated than meat.
) (66, 67, 68, 69). To consume enough protein, patients should be advised to consume fish, which is better tolerated than meat.
Simple sugar intake, especially added sugars (64), has been reported to cause dumping syndrome in as many as 76% (84) of the RYGB patients. The food rapidly enters the small intestine causing an osmotic load, which leads to movement of fluid from the blood into the intestine (85, 86). Rapid food entry into the jejunum also stimulates a substantial release of peptide hormones (85, 86). Clinical manifestations of the dumping syndrome include gastrointestinal symptoms such as early satiety, nausea, cramps, and explosive diarrhea and vasomotor symptoms such as sweating, flushing, palpitations, dizziness, and an intense desire to lie down (85). The insulin response is exaggerated and causes hypoglycemia (85, 86). To prevent dumping syndrome, patients should avoid consuming fruit juices and foods and drinks with added sugar (64); consume frequent, small, dry meals because water can make the food more soluble; include dietary fiber; increase dietary protein (especially fish and chicken); and modestly increase dietary fat (to delay gastric emptying) (86).
*************************************
Nobody is trying to make post-ops feel badly about their surgery choice. The DSers postings are aimed at pre-ops and potential revisions, to make sure they know about the DS BEFORE they choose which surgery to have. I'm sorry if that's how our postings make them feel, but that is not our intent.
We DSers also want people to know that we can help people with insurance issues, as most insurance companies can be FORCED to pay for the DS if the patient wants it and is willing to jump through the hoops to appeal -- one of the major independent medical reviewers in the country (used by many insurance companies and the federal government) TOTALLY supports the DS over the RNY when the IMRs are sent to them. Medicare changed their rules in 2006 (in no small part in response to a letter-writing campaign by us DSers!) to include the DS as a covered surgery. As more and more people stand up for their rights to have the surgery of their CHOICE, the insurance companies, one by one, are giving in and making the DS equally available, which is one of our major goals.
Dreamy
HW:303, SW:286, CW:148, GW:150
on 12/29/07 7:02 am
Learning about the DS? An excellent resource is www.dsfacts.com
For scientific studies about the DS and more, "friend" me, and then click on my profile. Best of luck on your journey.
~Link to my YouTube video blogs http://www.youtube.com/user/lorindablack
~ Picture instructions on how to make THE BEST protein shake EVER!!
~ More info on this amazing surgery at www.DSfacts.com (<--Link)
~Good info and links for pre-ops and newbies, click here
~Come hang out with the Indianapolis DS group -- calendar of events now online!
Duodenal Switch= Definite SOLUTION for Morbid Obesity!
HW:340 /SW:297 /CW:232 /GW:190 http://forgodsolovedme.com/
Revision Weight Loss Tracker  Mary
Mary

on 12/29/07 6:33 am
Hey Diana! Guess how long it took me to check out your profile since you've been back in OH town? Yup, I'm behind the 8-ball, for sure....just now! I HAVE to say...the pics of the wedding are FABULOUS, and what a GREAT IDEA to have the bridesmaids all wear black ****tail dresses! Talk about practical. I LOVE it. May I steal the idea for when/if I get married (again)? Loves, anne
Learning about the DS? An excellent resource is www.dsfacts.com
For scientific studies about the DS and more, "friend" me, and then click on my profile. Best of luck on your journey.





 Hear, hear! Let's all drink to Diana's BIG BRAIN! hehe! I'm glad you're putting it on your profile, Anne. I'll know where to find it when I need it that way!
Hear, hear! Let's all drink to Diana's BIG BRAIN! hehe! I'm glad you're putting it on your profile, Anne. I'll know where to find it when I need it that way!